Hackensack University Medical Center Continues to Lead Progress in Research, Technology and Techniques for Kidney-Sparing Surgery
3D imaging in the surgical suite improves outcomes with robotic kidney-sparing surgery
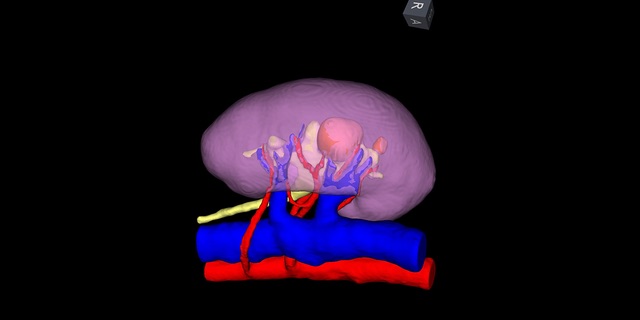
Hackensack University Medical Center is involved in five active research studies to assess risks, benefits and outcomes of robotic surgery and other novel technologies and procedures led by Michael D. Stifelman, M.D., Chair of Urology, Hackensack University Medical Center Director, Robotic Surgery, Hackensack University Medical Center that may be used in partial nephrectomies. Iris, a 3Dreconstructive imaging technology, is being used to plan and perform robotic partial nephrectomy surgeries on patients with high-complexity cancerous tumors even in a solitary kidney. Using data from diagnostic CT imaging, a segmented 3D model of a patient’s anatomy is created. This 3D anatomical representation platform makes it possible for surgeons to bring this 3D model into the operating and visualize it, manipulate and align it with the intraoperative view in real time within the surgeon’s robotic console. Research is underway to quantify the benefits.
HUMC has one of the largest prospective kidney cancer databases including surgical outcome data. Utilizing this prospective IRB database, Hackensack University Medical Center was able to assess the effect of experience on the incidence of postoperative arterial malformation and urine leak/urinoma after robotic partial nephrectomy. The overall incidence of postoperative complications after robotic partial nephrectomy remains low (5.3% vs 5.8%, overall: 5.6%). Urine leak and arterial malformation are becoming rarer with experience, despite increasing surgical complexity (0.55% vs 0%, 3.1% vs 1.1%).
Because the use of valve-less insufflation is gaining significant popularity for robotic partial nephrectomy, an investigative team also evaluated a valve-less trocar system (AirSeal), compared with conventional insufflation and the effects of insufflation pressure on perioperative safety outcomes. The study demonstrated that utilizing AirSeal (12mmHg pressure) provides a significant reduction in the incidence of subcutaneous emphysema compared to conventional insufflation (15mmHg) in patients undergoing robotic partial nephrectomy. In addition, the use of the AirSeal system at both 12mmHg and 15mmHg reduces postoperative shoulder pain compared with conventional insufflation. This suggests that for patients undergoing robotic partial nephrectomy, the use of AirSeal at 12mmHg provides the higher safety profile.
Other innovations that are improving outcomes in robotic kidney surgery include use of single port robotics, selective clamping, use of near infrared imaging and retroperitoneal access for tumors located anteriorly.
