An Astonishing Baby Delivery

November 13, 2019
Rosanna Aguilar and her husband, José-Luis, from Bluffton, South Carolina, were thrilled to learn they were expecting a third child. But elation turned to alarm at a routine ultrasound, when Rosanna learned that something was wrong with the placenta that could lead to severe bleeding.
Women with placenta abnormalities typically get blood transfusions during delivery. But that posed a problem. Rosanna, a Jehovah’s Witness, is prohibited from accepting blood or blood products. “Jehovah’s Witnesses view life as precious and seek out the best medical care available without the use of blood in obedience to God’s commands. We view of blood as representation of life,” she says.
Doctors hoped the issue would resolve itself without treatment. But as time went on, that possibility seemed less and less likely, and Rosanna sought help from a local high-risk OB/GYN. When they sat together in his office, the news was bleak. “I’m scared for you,” he told her. “Without a blood transfusion, your chance of survival is only 2 percent.”
Rosanna was unwilling to accept those odds. She contacted the Jehovah’s Witness Hospital Liaison Committee, who scoured the internet and made phone call after phone call, searching for someone who could help. Weeks went by, and six different hospitals refused to treat her. With each denial, Rosanna got increasingly frightened. She’d been told to deliver by 36 weeks to lessen the chance of serious bleeding. “I felt like a ticking time bomb. This baby was coming, and I couldn’t find anyone to help,” she says.
By 32 weeks, the Liaison Committee connected with Sharon Sledge, blood utilization coordinator at Hackensack University Medical Center. She directed Rosanna to Abdulla Al-Khan, M.D., director of Maternal-Fetal Medicine & Surgery and the Center for Abnormal Placentation at Hackensack.
A Turn for the Worse
Dr. Al-Khan agreed to meet with Rosanna. But when he examined her, he discovered the diagnosis was even more dire than her previous doctors had noted. Rosanna had placenta percreta, a rare condition where the placenta attaches itself and grows completely through the uterus. With this condition, the placenta doesn’t completely separate from the uterus after birth, which can cause life-threatening bleeding. In Rosanna’s case it extended into the bladder, making her condition even more perilous.
“This can be a long surgery that can result in a lot of blood loss,” says Dr. Al-Khan. “In a typical case I have a comfort level, knowing that in the event of significant bleeding, I can give a woman blood products and she won’t lose her life.”
But in this case, Dr. Al-Khan faced a considerable dilemma. As a physician, he’s taken the Hippocratic oath. But Rosanna’s religious belief forbids the very thing that will help. “So the question is, how do we balance my objective, which is to save life, and her need to follow her religion? How do we meet in the middle?” he says.
Doctor and patient had a candid discussion. Dr. Al-Khan asked Rosanna, “If the bleeding gets to the point of you dying, are you OK with that?” Rosanna responded, “I know that you’re going to truly give this your 100 percent, and that’s all I can ask of you. You’re respecting my wishes. So yes, I’m OK with that.”
Dr. Al-Khan agreed to do the surgery, which would be a C-section and partial hysterectomy to deliver the baby.
A Sleepless Night Before Surgery
The night before the surgery, Dr. Al-Khan agonized. “I was going through every step in my head. ‘What am I going to do if she bleeds here? What am I going to do if she bleeds there?’ And I admit, I was sweating. As a doctor, and as a human being, all I could think was, ‘I’m not sure I can handle a patient dying on me, knowing there’s something I can do to save her.’”
But Dr. Al-Khan and his team vowed to do everything in their power to prevent that result. They would use an approach called cell salvage to collect any blood she lost during surgery, which could then be recycled and infused back into her body. Almost 30 professionals made up the surgical team, including:
- a urologist to help with the bladder reconstruction
- a vascular surgeon who inserted balloons in arteries in her pelvis that could be inflated if needed to stem blood loss
- two anesthesiologists’
- a second maternal-fetal medicine surgeon
- obstetric and neonatal intensive care unit nurses
- a neonatologist
- operating room scrub technicians
- circulating nurses, and
- a perfusionist to run the cell salvage device.
Immediately before the procedure, Dr. Al-Khan gathered the entire team, including Jesus Rafael Alvarez-Perez, M.D., who assisted in the surgery. “We all had to understand that we were going to do every single thing to the best of our abilities to control the bleeding. But if we weren’t able to, we had to understand that this is the patient’s wishes,” he says.
Surgery lasted about seven hours, and Rosanna was awake the entire time to better help minimize blood loss. “It was magnificent. I could hear Dr. Al-Khan giving the commands the entire time. He just ran that OR like a superstar,” she says.
An Astonishing Delivery
Dr. Al-Khan and his team delivered the baby first. Then the real work began:
- Al-Khan had to remove Rosanna’s uterus, methodically cauterizing and tying each artery and vein.
- Then he and the urologist systematically dissected the bladder from the uterus without causing excessive bleeding.
- Finally, the uterus, with the placenta firmly attached to it, was removed successfully.
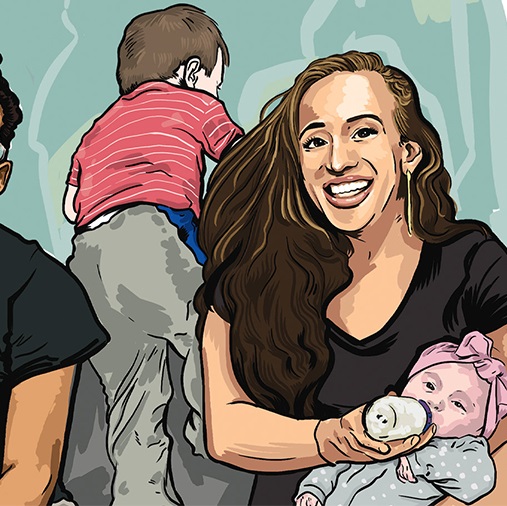
Miraculously, Rosanna only lost about 100 cc of blood. Typically with placenta percreta surgeries, blood loss is between 3,000-3,500 cc, according to published data. After a few hours in recovery, Rosanna was thrilled to hold her baby boy. “I am so incredibly grateful to Dr. Al-Khan,” she says. “Without him, I don’t think I’d be here.”
The material provided through HealthU is intended to be used as general information only and should not replace the advice of your physician. Always consult your physician for individual care.
From the NICU to Thriving at Home

In the spring of 2019, Sarah Garland and Keith Wallenstein were eagerly awaiting the birth of their first child. With three months to go before the August due date, they were still debating names.

Delivering a Baby While COVID-Positive
When Maria Acevedo opened her eyes on March 31, 2020, she was in a hospital bed, surrounded by baby photos taped to the walls. So much had changed in the four days she had been asleep.

Change of Birth Plans
As the old saying goes, the best laid plans often go awry. Sometimes that’s unfortunate; other times it’s serendipitous. Thankfully for Dena and Yaakov Kibel, it was the latter.

At the Ready for an At-Risk Birth
Suzanne Hahl, age 40, sat down to relax in her Middletown, New Jersey, home after celebrating her son’s first birthday when she started to feel a little odd.
Fighting for Two: COVID-19 and Pregnancy
By the time Donna Molina sniffed a bottle of bleach and couldn’t detect its odor, she knew: She had Covid-19.