
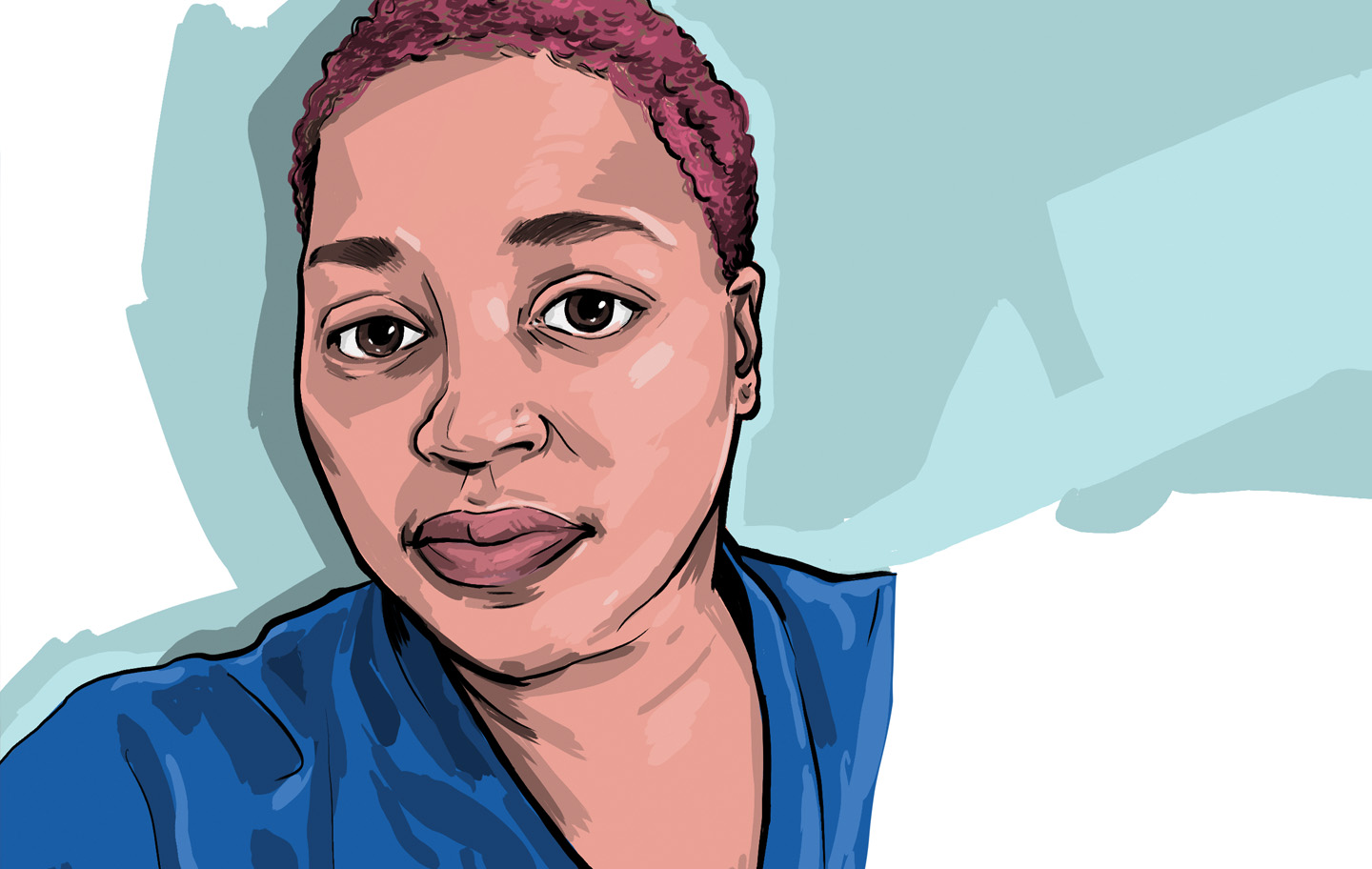
It was a hot summer day in June 2019, and Christina Hunter-Carey, 47, from Piscataway, New Jersey, laced up her sneakers. She had taken a quick nap after she got home from work as a learning disabilities consultant, so she was running late for her date with a treadmill and free weights.
“I jumped up and my legs gave out from under me,” she says. She blacked out for a bit, then managed to pick herself off the floor and call her husband. He raced home, and together they rushed to the nearest hospital.
Doctors diagnosed a transient ischemic attack (TIA), also known as a mini stroke, a stroke that lasts only a few minutes. An MRI revealed that Christina had moyamoya, a rare condition that puts people at higher risk of a stroke. A month later, Christina needed another surgery, which led to a second stroke, this one far more debilitating.
When she woke up, Christina was unable to move her right arm or right leg. The only word she could utter was “no.” “I was overwhelmed,” Christina says. “This wasn’t supposed to happen.”
Soon after her stroke, Christina started rehabilitation at the Brain Trauma Unit at JFK Johnson Rehabilitation Institute. “We’re part of an acute care hospital that includes a leading neuroscience institute, so we’re able to treat patients who have both complex brain injuries and complex medical problems because of the resources we have at our fingertips,” says Brian D. Greenwald, M.D., medical director of the Center for Brain Injuries at JFK Johnson.
Dr. Greenwald assured Christina that she would be well taken care of. “What’s unique about our program is that our continuity of care allows us to keep what I call the ‘warm hug’ on people until we get them better,” he says.
Moving On
Christina began working with a team of therapists, eventually receiving at least three hours of intense daily therapy. While her speech came back fairly quickly, physical strength was tougher.
“One day, my physical therapist, Shannon, tried to get me to walk upstairs, and I couldn’t do it,” she says. “I just cried and said, ‘I’m never going to walk again.’”
But her physical therapist refused to let Christina give up. “She told me, ‘It’s going to be hard work, but I promise, you will be able to walk again,’” Christina recalls.
Within a few weeks, that promise was kept. “She put me in a contraption with belts holding me up, and I was able to make it to the end of the hallway and back. It felt so good to accomplish that,” Christina says.
Within a month, Christina transferred to the nearby JFK Hartwyck at Oak Tree, the only state-certified subacute brain injury rehabilitation program in New Jersey, under the care of Jaime Levine, D.O., medical director of brain injury rehabilitation at the Extended Recovery Unit at JFK Johnson.
While Christina would have preferred to go straight home, she needed more time under the care of a team familiar with brain injury. “We agreed that she belonged at home,” Dr. Levine says. “But we had to make sure she’d be safe when she got there.”
Christina continued to work on physical strength as well as cognitive, communicative and functional goals. Speech therapists used a metronome to help her speak more fluidly. Recreational therapists took her to the grocery store to help her with shopping. “It was the first time I used a mobile shopping cart, and I had to learn to maneuver it like when I first learned to drive a car,” Christina says.
While she continued to progress physically, the emotional turmoil could be difficult, so the team added group therapy to her routine. “Connecting with others going through the same things made me feel less alone,” she says.
The team described how throughout Christina’s therapies, her brain needed time to adjust and reconnect with various parts of her body. “They explained the concept of neuroplasticity—the brain’s ability to rebuild itself—which reassured me that the work we were doing would help me recover,” Christina says.
Home, Sweet Home
About a month later, Christina was discharged. Therapy continues even today. “While big changes come in the first few months, a patient like Christina who is dedicated to performing her home exercise program can expect continued improvement in her strength and quality of movement for an extended period of time,” says Steven Escaldi, D.O., medical director of the Spasticity Management Program and attending physiatrist at JFK Johnson.
Christina receives therapy at home, including physical, occupational and counseling services, through the Outpatient Cognitive Rehabilitation Department. She’s doing exercises and receiving botulinum toxin injections to relieve stiffness and muscle spasms. She continues to fine-tune the skills she learned during her inpatient rehabilitation.
Today, Christina considers her progress nothing short of miraculous. “When this all started, I felt like I was going to be an invalid,” she says. But she’s far from it. Christina’s back at work, and not only is she walking—on her own—2 miles a day, she’s even running. She plans to complete a beginner race with her therapy team in 2021.
My therapists have become family,” Christina says. “They got to know me as a person, not just a patient in room 101. They literally put me back together, physically, mentally and emotionally. I will be forever grateful.”
Next Steps & Resources
- Meet your sources: Brian D. Greenwald, M.D., Jaime Levine, D.O., and Steven Escaldi, D.O.
- To make an appointment with Brian D. Greenwald, M.D., Jaime Levine, D.O., Steven Escaldi, D.O. or another provider, call 800-822-8905 or visit our website
Find a doctor near me

Do Over-the-Counter Knee Braces Help?

Five Tips for a Healthier Workout

How to Identify Early Signs of Stroke
