JFK Johnson’s Expanded Spinal Cord Injury Program: Advancing What’s Possible
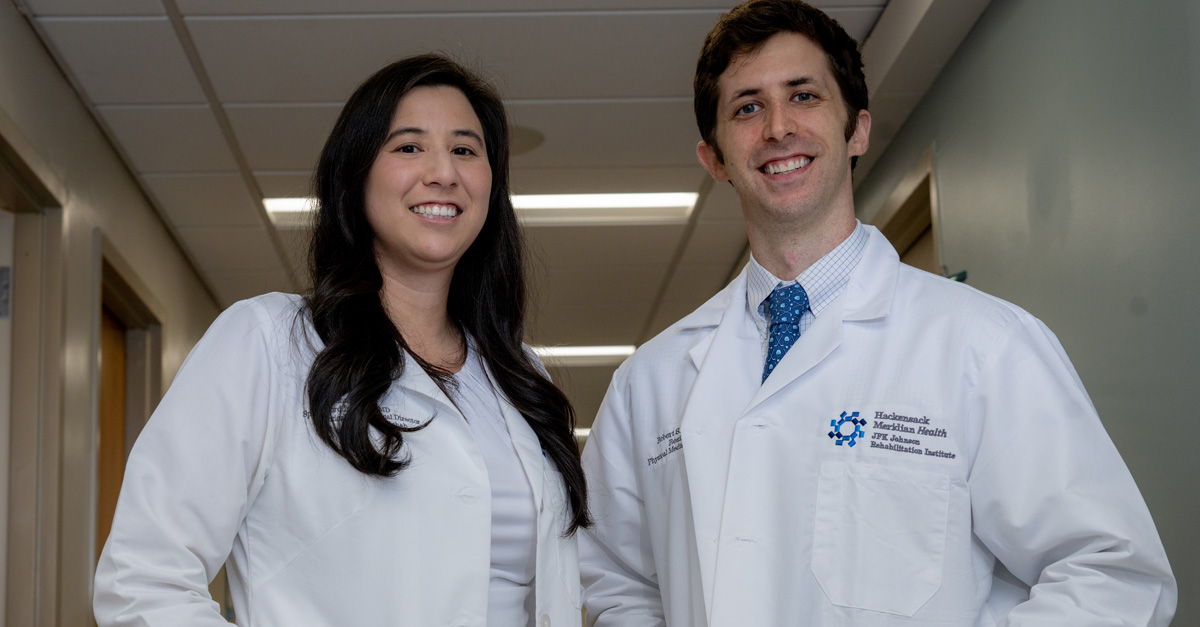
JFK Johnson Rehabilitation Institute continues to expand its Spinal Cord Injury Program, bringing new expertise, research, and technology to meet the complex needs of patients. Led by board-certified rehabilitation physicians Jennifer Chui, MD, and Phillip Gordon, MD — both subspecialists in spinal cord injury medicine — the program provides the full spectrum of care for patients living with these life-changing injuries.
JFK Johnson’s multidisciplinary team works to prevent complications, promote healing, and help patients regain independence. “My goal is to help patients regain everything that’s possible — and to adjust to a new normal while maintaining the best quality of life,” says Dr. Chui. Adds Dr. Gordon, “We make sure each patient has a chance to tell their story, and we regularly ask, ‘What are your goals?’”
Every patient undergoes a thorough evaluation and receives a customized treatment plan by a team led by a physician specializing in spinal cord injury medicine. The team can include nurses, physical and occupational therapists, social workers, psychologists, and others with experience in spinal cord injuries. For some, care can begin at the dedicated spinal cord injury unit, such as the Eric LeGrand Spinal Cord Injury Patient Care Room, named after the Rutgers University football player who was injured during a game.
Social workers also support patients through insurance navigation, community reintegration, and long-term planning. The team conducts family meetings and education sessions to support patients as they transition to home and continue with outpatient therapy and treatment.
Advanced technology and focused treatment
Patients, both in- and out-patient, can benefit from a range of resources, including:- ZeroG® Gait and Balance System, a body-weight support system.
- Exoskeleton Technology, a wearable robotic suit used for gait training, giving patients with incomplete injuries an opportunity to strengthen mobility.
- Functional electrical stimulation (FES) bikes, which use electrodes to activate weakened or paralyzed muscles in patients seated in wheelchairs.
- LiteGait, a partial weight bearing device to assist patients in walking, balance, and posture.
- Specialty clinics, such as those on spasticity management, pelvic floor therapy, wheelchair skills, and prosthetics and orthotics.
- Driver training with adaptive hand devices.
- Treatment from psychologists with experience in rehabilitation medicine and spinal cord injury.
“Our new technologies and resources are benefiting our patients as we work to help them gain mobility and independence,” said Cynthia Thomas, PT, DPT, NCS, a Board-Certified Neurologic Clinical Specialist. Her job, she says, requires problem solving and creativity as she works to enable patients to return to doing the things they love — a role that is both challenging and rewarding.
“We have the opportunity to have such an impact on the lives of our patients,” Thomas says. “We see where they start and how much they progress.”
Kelly N. Scimeca, MS, OTR/L, who has worked with spinal cord injury patients for nearly a decade, provides wheelchair skills and body positioning techniques, as well as helping patients find the right wheelchair — perhaps an ultralight wheelchair or maybe a motorized device. As an occupational therapist, she also helps patients learn new ways to be independent, such as getting themselves bathed and dressed.
“We help people gain confidence,” Scimeca says. “I am always impressed with the resilience of our patients who are dealing with a devasting and lifelong impact in their lives. I often see resiliency emerge that people did not know they had.”
Industry leadership
At JFK Johnson, the approach is whole-person-centered. Dr. Chui and Dr. Gordon compare the brain to a computer and the spinal cord to the wiring that carries signals to the body. When that wiring is damaged, the consequences ripple everywhere.
“Many providers don’t fully understand how broad the impact is — from heart and lung function to bladder, bowel, and sexual health,” Dr. Chui said. “Everything needs to be addressed.”
Variation among patients can be far-reaching. “It’s not simply, ‘You’ll never walk again,’” Dr. Chui explains. “Some injuries are incomplete, and patients may regain significant function. Even some complete injuries can convert to incomplete.”
The goal is independence and mobility, whether that is walking, walking with specialized devices, or mastering a wheelchair. Some patients find new ways to enjoy sports, says Gordon, who has a focus on adaptive sports, such as adaptive surfing on the Jersey Shore.
“We work to maximize each patient’s functional gains and their chances of healing,” Dr. Gordon says. “Our patients are on a physical, mental, emotional, and spiritual journey.”
Leadership in Care for Women
The expansion highlights JFK Johnson’s leadership in specialized care for women with spinal cord injuries, an often-underappreciated area. Dr. Chui recently co-authored, Rehabilitation Considerations for Women with Spinal Cord Injury, an article that provides national guidance to health care providers to improve the treatment of women. The article is part of a special issue of the international medical journal, Physical Medicine and Rehabilitation Clinics, that explores issues surrounding women and rehabilitation medicine.
“The goal of the article is to help health care providers recognize and address the specific care points for women,” Dr. Chui said.
Dr. Chui also serves as one of the editors of the spinal cord injury section of Physical Medicine and Rehabilitation Board Review, the PM&R review book used by medical students, residents, fellows, and attendings around the nation who are seeking board certification in rehabilitation medicine. Sara Cuccurullo, M.D., Medical Director of JFK Johnson, serves as editor of the book, now in its fifth edition.
As an academic rehabilitation hospital, JFK Johnson physicians, researchers, fellows, and medical students routinely engage in research across rehabilitation medicine, including spinal cord injury. Current research at JFK Johnson aims to enhance quality of care for spinal cord injury patients who are undergoing inpatient rehabilitation. Current research endeavors focus on factors that influence the length of hospital stays, with the objective of reducing both the duration of hospitalization and potential complications that may occur among patients with spinal cord injuries.
Range of Causes of Spinal Cord Injuries
Dr. Chui and Dr. Gordon care for patients with traumatic spinal cord injuries, such as those in sudden accidents, including car crashes, as well as falls, sports injuries, or acts of violence. Traumatic injuries can often be simple slips and household accidents. Other times, the cause is a health condition. For example, tumors, infections, strokes of the spinal cord, or diseases such as multiple sclerosis can damage the spinal cord. Dr. Chui and Dr. Gordon have made helping all these patients the main focus of their medical careers. “We often see good recoveries, and, with other patients, we make a remarkable improvement in the quality of their lives. It’s immensely rewarding to be a part of that,” says Dr. Chui. Dr. Gordon notes a phrase he recalls from his Jesuit Catholic high school in Philadelphia: cura personalis, a Latin phrase that translates to "care of the whole person.” Dr. Gordon says the desire to bring that principle to medicine “drew me to this specialty. You make a difference in the lives of your patients.”
Learn more about our innovations in rehabilitation care.
If you are a patient looking for expert rehabilitation care at Hackensack Meridian Health, please visit our rehabilitation services page to learn about our specialties, find locations, and schedule appointments.
