Bariatric Surgery Vs. GLP-1: Which Weight Loss Option Fits You?

January 26, 2026
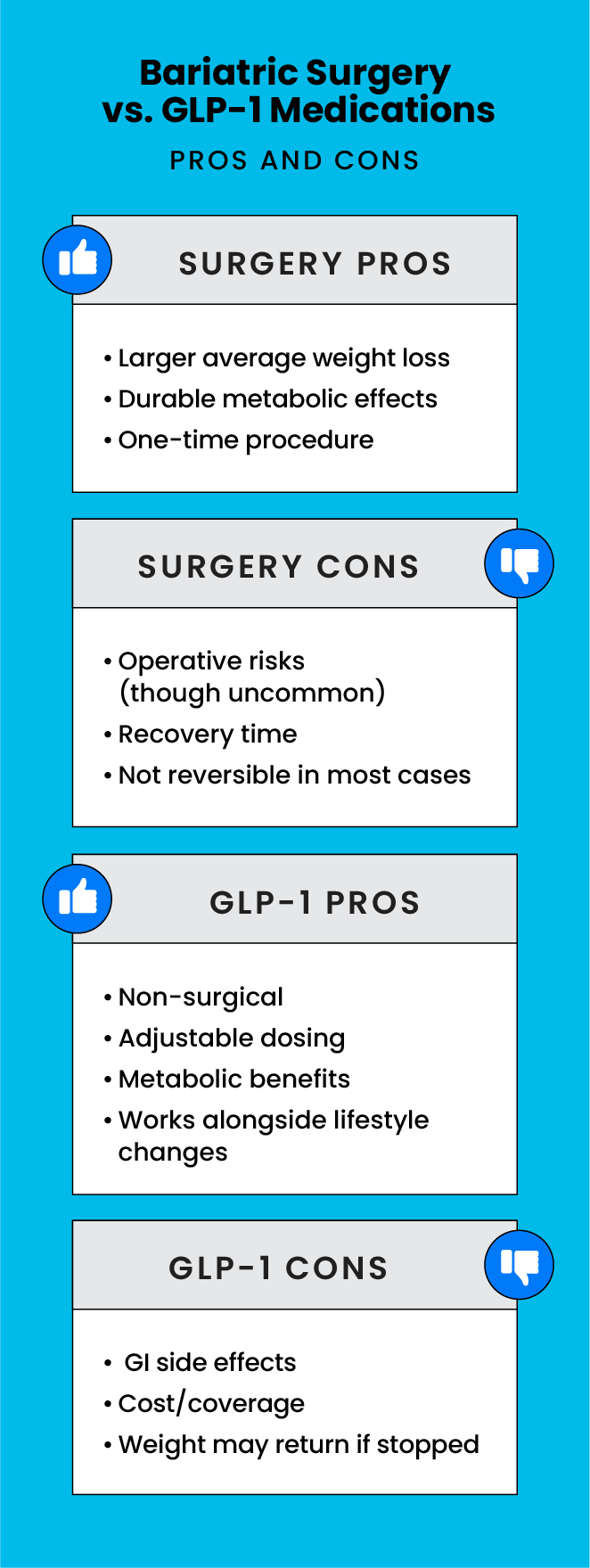
If you’ve made meaningful changes to diet, exercise and lifestyle but still aren’t seeing the weight loss results you need, you may be wondering what the next step should be. Bariatric surgery and GLP-1 medications are two evidence-based options your care team may discuss with you if you have a higher body mass index or BMI, or if you have weight-related health conditions such as type 2 diabetes.
As you’re considering your options, it’s important to understand that obesity is a chronic medical condition — not a willpower issue. Many people need medical or surgical support to reach a healthier weight. We spoke with Seth Kipnis, M.D., a board-certified general surgeon and Medical Director of Bariatric and Robotic Surgery at Jersey Shore University Medical Center, and Ritu Anand, M.D., a board-certified endocrinologist at the Center for Weight Loss at JFK University Medical Center, to explain how bariatric surgery and GLP-1’s work, who they’re best for, and what to expect — so you can discuss the next right step with your care team.
Who Might Benefit from Each Option?
Bariatric surgery may be a good fit for adults with higher BMI and obesity-related conditions who are ready for a procedure and ongoing nutrition support, including daily vitamin and mineral supplements and periodic lab checks to make sure nutrient levels stay healthy.
Bariatric Surgery May Be a Good Choice If You:
- Meet surgical criteria (a BMI of 40 or higher, or a BMI of 35 or higher with a weight-related condition like type 2 diabetes, sleep apnea or high blood pressure) and have obesity-related health conditions
- Want a one-time procedure with structured follow-up
- Are comfortable with permanent anatomy changes and lifelong supplements
GLP 1 medications may be a good fit for adults who prefer a non-surgical path, can take medication as prescribed with regular monitoring and meet clinical/insurance criteria.
GLP 1 Medications May Be a Good Choice If You:
- Can take medication as prescribed with regular monitoring and meet medical criteria —usually a BMI of 30 or higher, or 27 with conditions like type 2 diabetes, high blood pressure or high cholesterol
- Prefer a non-surgical option and can commit to regular use and follow-up appointments
- Understand that stopping medication may lead to weight regain without continued lifestyle support
Understanding Bariatric Surgery and GLP-1 Medications
Still not sure what’s right for you? Learning more about each weight loss option can help you make an informed decision, alongside your doctor.
What is Bariatric Surgery?
Bariatric surgery changes the stomach and/or intestines to support meaningful, long-term weight loss and improve health conditions such as type 2 diabetes, sleep apnea and high blood pressure. Most procedures are minimally invasive and include careful preparation and follow-up.
Bariatric surgery includes several procedures that help with weight loss and overall health:
- Sleeve gastrectomy: Removes part of the stomach to reduce hunger and food volume.
- Gastric bypass: Creates a smaller stomach pouch and reroutes the intestines to change hunger hormones and absorption.
“Sleeve surgery is the most common – it’s simpler, recovery is easier and results are durable for many people,” says Dr. Kipnis. “We usually reserve gastric bypass for patients who need to lose more weight or have had prior operations.”
Who Should Get Bariatric Surgery?
“Doctors use BMI as a starting point – plus any weight-related health issues – to match you with medicine, surgery or both,” says Dr. Kipnis. “Many plans cover surgery because, for many people, the long-term risks of staying at a higher weight are greater than the risks of modern surgery.”
You may qualify for bariatric surgery if:
- Your BMI is 40 or higher.
- Your BMI is 35 or higher and you have a weight-related health condition such as diabetes, high blood pressure, sleep apnea or fatty liver disease.
- You’ve tried medically supervised lifestyle changes without enough improvement.
How Can Bariatric Surgery Help?
- Meaningful weight loss and improvement in conditions like type 2 diabetes, sleep apnea and high blood pressure
- More energy for work, family and movement
- Long-term support for weight maintenance when paired with healthy habits
“Within weeks, many people need fewer medications, sleep better and move with less pain,” says Dr. Kipnis. “Diabetes and blood pressure drugs are often reduced or tapered as your health improves.”
What Are GLP-1 Medications?
GLP-1 medications (injections or pills) are taken under a doctor’s guidance and can help control appetite and blood sugar. “GLP-1 medications act like a natural gut hormone,” explains Dr. Anand. “They quiet ‘food noise,’ so appetite goes down and you feel full with less food.”
Results vary from person to person, but most people in clinical trials lose about 15-21 percent of their starting weight.
How Can GLP-1 Medications Help?
- Clinically significant weight loss for many people while on the medicine
- Better metabolic health, including improved A1c (a blood test that shows your average blood sugar level over the past two-to-three months), blood pressure and cholesterol for appropriate patients
- A non-surgical approach you can start with medical supervision
Combining Bariatric Surgery and GLP-1s
Some people use GLP-1 medications before surgery to improve readiness (i.e., better control over conditions such as diabetes) and after surgery to manage plateaus or weight regain. “We use every safe tool that works – GLP-1 medications and, when appropriate, surgery – so patients don’t have to pick one path too early,” says Dr. Kipnis. Dr. Anand adds, “We start low and go slow with GLP-1 medications and check in regularly – our goal is steady, safe progress that protects your health and can work alongside surgery when it’s the right fit.”
Safety: What About Risks and Side Effects?
Bariatric Surgery:
Surgery is very safe, but like any operation, it has risks. Rare problems include bleeding, a leak from where the stomach or intestines were joined, a narrowing (scar tissue) that makes food harder to pass and blood clots. Long term, your body absorbs nutrients differently, so you’ll need daily vitamin and mineral supplements to keep your levels healthy. Your medical team will explain how they prevent, detect and treat these issues and will give you a clear nutrition plan. “For many patients, the long-term health risks of staying at a higher weight are greater than the risks of modern bariatric surgery,” says Dr. Kipnis. “This is why many insurers cover it when criteria are met.”
GLP 1 Medications:
Common side effects include nausea, fullness and constipation. These often improve with slow dose increases. Your clinician will review important safety considerations, such as a history of pancreatitis, gallbladder issues or certain thyroid conditions, to ensure these medications are safe for you. “Some people should avoid these medications depending on medical history,” says Anand.
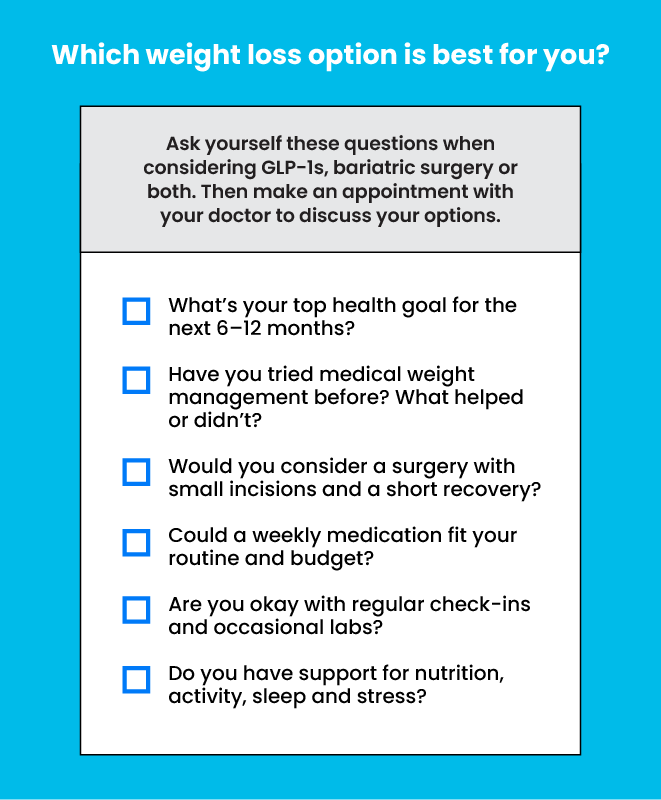
Next Steps & Resources
- Meet our sources: Seth Kipnis, M.D. and Ritu Anand, M.D.
- Make an appointment online or call 1-844-HMH-WELL.
- Find a bariatric specialist or endocrinologist specializing in weight loss near you.
- Learn more about bariatric surgery and GLP-1 programs at Hackensack Meridian Health.
The material provided through HealthU is intended to be used as general information only and should not replace the advice of your physician. Always consult your physician for individual care.








