Just Like New After Cardiac Stents
January 24, 2021
Typically, we photograph every patient appearing in HealthU. Because this story was planned during the surge of COVID-19, that contact would have been too risky. Instead, our team took a creative approach and replaced photo shoots with illustrated portraits of patients.
In April 2017, Mike Fleming, 61, of Hazlet, New Jersey, was at the candle factory where he has worked for 15 years as an electrical and mechanical engineer when he felt a terrible pain on his left side. His initial thought was that he was just constipated and it would pass.
He’d had a bout of bad constipation just four months earlier, and this felt similar. “I’m figuring I’m constipated again,” he says. “I’m like, this really stinks.” He powered through the discomfort until lunchtime, when a co-worker told him he looked horrible and had lost all the color in his face.
Mike brushed it off and told his co-worker he’d take a half-hour nap at lunch, but his co-worker persuaded him go to a nearby emergency department, where he learned the pain was being caused by kidney stones.
In addition, a cardiologist appeared at his bedside to inform him he also had an unrelated abdominal aortic aneurysm. The bulge in the largest blood vessel in his body wasn’t so big that he would need emergency treatment, but he would need regular checkups to keep tabs on its growth.
His regular checkups took a backseat to a hip surgery, so when he finally had his aneurysm checked again in late 2019, he found out it had grown to a point that it needed to be addressed. He also needed several cardiac stents to manage blocked arteries.
Best Things Come to Those Who Wait
Mike was supposed to get his blocked arteries and growing aneurysm taken care of in February and March 2020, but then COVID-19 hit New Jersey hard and everything that wasn’t an emergency was put on hold due to government restrictions.
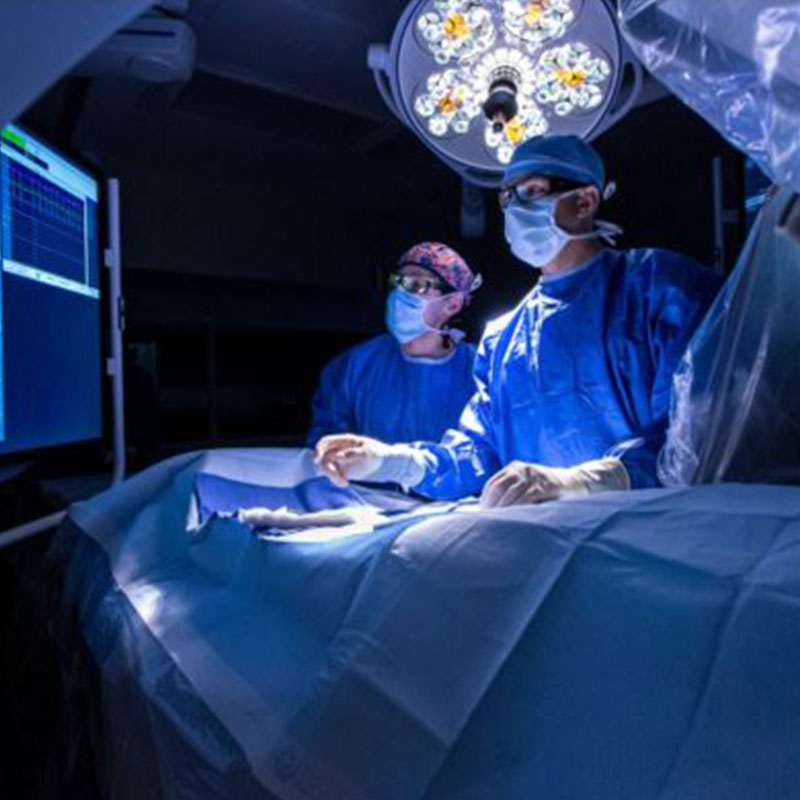
He was able to meet Habib U. Khan, M.D., his new vascular surgeon at Bayshore Medical Center, via a telehealth appointment and discuss what to do about his abdominal aortic aneurysm. The aneurysm, Dr. Khan says, was in a tricky spot: close to the arteries that branch off the aorta to Mike’s kidneys.
Traditionally, to treat an aneurysm like this, Mike would have to undergo an open surgical procedure, which would involve a large incision on his stomach, a few days’ stay in the intensive care unit and a period of in-hospital rehabilitation before being able to go home. But due to Dr. Khan’s advanced endovascular skill set and the possibility of an FDA-approved fenestrated abdominal aortic aneurysm graft, patients like Mike have options that involve less risk and reduced recovery time.
A fenestrated abdominal aortic aneurysm graft is a custom-designed stent-graft that has openings to match the specific locations of a person’s kidney and intestinal arteries. A CAT scan is taken of the area where the stent-graft will go. The device manufacturer uses a model based on the scanned area to create a stent-graft that is custom-fit to the patient. Mike’s custom stent-graft was manufactured in Australia by a U.S.-based medical device company.
“When the stent is within the aneurysm, it keeps all the blood flow within the stent. So there’s no chance of the aneurysm leaking or rupturing,” says Dr. Khan, adding that the multiple openings allow blood to flow through the stent-graft into the arteries that branch off the aorta.
Because of Mike’s heart disease and recent cardiac stents, he wasn’t a good candidate for traditional open surgery. But he was a great candidate for a fenestrated endovascular aortic repair, or fEVAR.
Unlike a traditional open surgical procedure, fEVAR doesn’t require a large incision—usually it takes just two small incisions in the groin, but sometimes no incision is needed at all, Dr. Khan says. Because the procedure is minimally invasive, patients can go home in a day or two and don’t require rehabilitation.
The fEVAR procedure was approved by the FDA a few years ago, so only a handful of hospitals in New Jersey have been offering it. When Mike had his fEVAR procedure in August 2020, it was the first time the procedure was performed at Bayshore.
“In the past, all of these complex aortic aneurysms would be referred to other hospitals,” Dr. Khan says. “But now they can safely be done at Bayshore.”
Fixer-Upper
Mike was able to go home the day after his fEVAR procedure. He had swelling in his groin area, but other than that, he’s felt good—so good, in fact, that he spent much of his recovery reconditioning a pickup truck he’d recently purchased.
“You’ve got to exercise. You’ve got to work your way up to it. While I was home, I reconditioned my truck from front to back,” he says. “I put in shocks, brakes, rotors, calipers, tune-ups, spark plugs. My truck is like brand new.”
Now with replaced hips and a few stents in his body, Mike feels a bit like an old truck that’s been reconditioned. “I’ve always said a doctor is like a mechanic. Mechanics work on cars; doctors work on bodies,” he says. “A body is just a little more complicated.”
Next Steps & Resources
- Meet your source: Habib U. Khan, M.D.
- To make an appointment with Habib U. Khan, M.D. or another provider, call 800-822-8905 or visit our website
The material provided through HealthU is intended to be used as general information only and should not replace the advice of your physician. Always consult your physician for individual care.
After a Serious Cardiac Condition, Where is She Now?

In 2018, we shared the story of Emer Featherstone, who was rushed to the emergency department at Mountainside Medical Center when extreme fatigue turned out to be a serious cardiac condition.

After Experiencing an Aortic Aneurysm, Where is He Now?
In 2018, we shared the story of Thomas Redmond who was nicknamed “the healthiest man in the ICU”.

After a Heart Attack in His Thirties, Where is He Now?
In early 2020, we shared the story of Przemyslaw “Simon” Blazejowicz, whose life hung in the balance as doctors at JFK Medical Center rushed to unravel the medical mystery that led to his heart attack...
Big Heart, Big Fix
Attorney Gerald Dienst was diagnosed with congestive heart failure and atrial fibrillation in 2012. Today, a remarkable new device is reducing his risk of blood clots and stroke, and ensuring he can continue helping his clients.
Life After Bypass
When Jeffrey Wells woke up one Saturday morning in August 2020 feeling “like an elephant was on my chest,” the retired police officer’s first inclination was to relax and wait a few minutes until he felt better.