Hackensack University Medical Center Is a Leader in Multiple Myeloma Treatment
John Theurer Cancer Center, part of Hackensack University Medical Center, is one of the largest providers of myeloma services in the world with over 20,000+ myeloma specific visits per year
Under the leadership of David Siegel, M.D., Ph.D., David Vesole, M.D., Ph.D. and Noa Biran, M.D. and Harsh Parmar, M.D., the Multiple Myeloma (MM) Division at John Theurer Cancer Center, part of Hackensack University Medical Center, is driving innovation in precision medicine and advanced immunotherapeutics. The providers of the MM program care for over 2,000 patients, half of whom are on active therapy, and follow patients longitudinally from diagnosis. The program brings a unique world-class, state-of-the-art academic approach together with a community feel and patient-focused care.
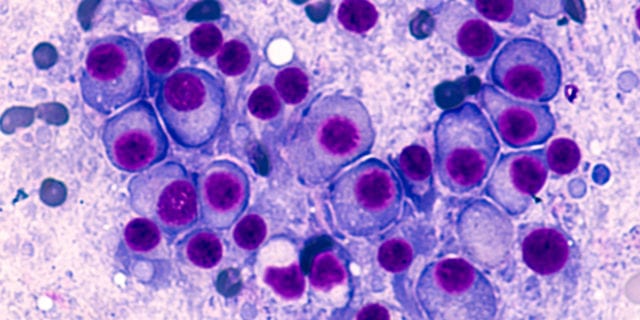
The myeloma division at JTCC completes on average 250 stem cell transplants for multiple myeloma patients each year. It is also the second largest enroller of patients in the CoMMpass study, and the Multiple Myeloma Research Foundation’s (MMRF) Personalized Medicine Initiative, built on new genome sequencing technologies. There is also high-level integrative collaborative efforts with the Center for Discovery and Innovation as part of the Hackensack Meridian School of Medicine and with our NCI Comprehensive Cancer Center affiliation with Georgetown Lombardi Comprehensive Cancer Center. Research for this division has been recognized in publications such as The New England Journal of Medicine, Journal of Cancer Oncology, The Lancet Haematology and Blood. Recent findings follow.
- The role of CAR T-Cells in the management of relapsed and newly diagnosed myeloma.
- The role of monoclonal antibodies in combination with proteasome inhibitors in the treatment of myeloma.
- BCMA as a target for the treatment of myeloma. This can be approached using a number of modalities such as monoclonal antibodies, antibody drug conjugates, CAR T-cells, T-Cell engagers (bispecific antibodies). A study of chimeric antigen receptor (CAR T) cells in relapsed/refractory MM targeting the B cell maturation antigen (BCMA) demonstrated that heavily pretreated patients the objective response rate was 85%, including 45% complete responses. This has led to a series of other BCMA-directed CAR T trials including the KARMMA-2 trial which has been submitted to the FDA for CAR T-Cell approval.
- Part of the approval process for the most recently approved drugs, isatuxumab, selinexor and belantamab.
- A number of studies on the proteasome-inhibitor, carfilzomib, demonstrating efficacy of once weekly compared to twice weekly administration and with once weekly carfilzomib with lenalidomide and dexamethasone have been complete in both newly diagnosed MM as well as relapsed MM showing safety and efficacy.
- Participating in clinical trials with therapeutic NK cell products, new derivatives of thalidomide as well as a large number of other new modalities. Over 30 clinical trials accruing pts with multiple myeloma, including more than a dozen cellular therapeutics and other novel modalities.
- A study of 437 patients with MM treated with selinexor – an oral, small molecule inhibitor of the nuclear export protein exportin 1 with demonstrated activity in hematologic and solid malignancies – assessed the kinetics of adverse events and impact of supportive care measures. Selinexor reduced both platelets and neutrophils over the first cycle of treatment and reached a nadir between 28 and 42 days. Platelet transfusions and thrombopoietin receptor agonists were effective at treating thrombocytopenia, and granulocyte colony stimulating factors were effective at resolving neutropenia. Selinexor has well-established adverse effects that mainly occur within the first 8 weeks of treatment, but they are reversible, and respond to supportive care.
- There is evidence for B-cell maturation antigen expression in various hematologic malignancies, suggesting that BCMA may play an important role as a biomarker or therapeutic target in these diseases. Given advances in understanding the role of BCMA in B-cell development and the promise of BCMA as a therapeutic target, John Theurer Cancer Center conducted a systematic literature review of publications reporting BCMA expression in patients with hematologic malignancies. The team’s results suggested that BCMA is a relevant target in MM as well as in a subset of B-cell leukemia.
Learn more about advances in oncology care happening at Hackensack University Medical Center.

