Urogynecology
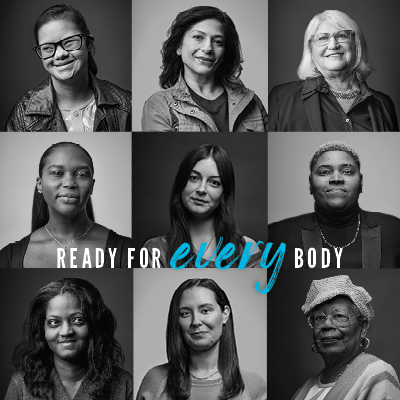
Pelvic floor and bladder disorders can become more common with age, but you don't have to live with the discomfort. If you're experiencing symptoms like pain in your lower abdomen, pelvic pressure, or changes in bladder, bowel, or sexual function, our specialists at Hackensack Meridian Health are here to help.
We provide advanced, patient-centered urogynecology care for women across New Jersey, with expert teams in North, Central, and South NJ, so you can find compassionate care close to home. As part of one of the state's largest health networks, we combine clinical expertise with minimally invasive options to help you regain your comfort and quality of life.
When to See a Urogynecology Specialist
Our urogynecologists treat common gynecologic conditions, such as:- Bladder pain (not related to infection)
- Dropped pelvic organs
- Frequent urge to urinate
- Inability to completely empty the bladder
- Loss of bladder control
- Pain during sexual intercourse
- Sense of fullness, pain or pressure in the pelvis (not related to infection)
- Vaginal pressure or bulging
Specialized Treatments for You
Urogynecologists at Hackensack Meridian Health are fellowship trained in Female Pelvic Medicine and Reproductive Surgery. They offer the full range of treatments and surgeries to help you return to a more comfortable and active lifestyle. Your condition may be resolved without surgery using:- Changes to your diet
- Medication or injections
- Nerve stimulation and implanted devices
- Pelvic floor or bladder strengthening exercises
If surgery is required, our urogynecologists are leaders in the New York/New Jersey metro area in minimally invasive and robotic surgeries. We can recommend the best approach to repair your pelvic floor or bladder condition.
Pelvic Floor Disorders
Overview
A pelvic floor disorder is the dropping of your bladder, rectum, or uterus due to weakness of the muscles and supporting tissue. If the condition is severe, tissues may even protrude outside the body.
Symptoms of a Pelvic Floor Disorder
- Feeling of heaviness or pressure in the vagina
- Feeling that the uterus, bladder, or rectum is dropping down
- Painful sexual intercourse
Types of Pelvic Floor Disorders
Pelvic floor disorders are basically hernias, in which tissue protrudes because another tissue is weakened. Women may have more than one pelvic floor disorder at the same time, including:
The bladder drops down and protrudes into the front wall of the vagina. A cystourethrocele is when the upper part of the urethra also drops down.
Common Symptoms: passing urine when coughing, sneezing or laughing; passing urine when the bladder becomes too full; the bladder may not feel completely empty; or an intense urge to urinate
The small intestine and the lining of the abdominal cavity bulge between the uterus and the rectum or, if the uterus has been removed, between the bladder and rectum.
Common Symptoms: fullness, pressure or pain in the pelvis
The rectum drops down and protrudes into the back wall of the vagina.
Common Symptoms: difficult bowel movements, sense of constipation
The uterus drops down into the vagina.
Common Symptoms: pain in the lower back or over the tailbone, difficult bowel movements
Diagnosis
Your urogynecological specialist can typically diagnose any potential Pelvic Floor Disorders you may have by performing any of the following methods:- Flexible viewing tube to see inside the bladder (cystoscopy)
- Urine tests
- Physical exams
Treatment Options
- Estrogen vaginal suppositories and creams
- Kegel exercises to strengthen the pelvic floor muscles
- Pelvic floor reconstructive surgery
- Pessary device inserted into the vagina to support the pelvic organs
Pelvic Floor Reconstructive Surgery
For some instances, reconstructive surgery may be necessary to treat prolapses of the uterus, rectum, bladder and vagina. These surgical procedures are typically minimally invasive, with only a few small incisions made in the vagina and pubic line. Following surgery, patients generally are required to spend several days in the hospital and may fully recover within two weeks.
Bladder Disorders
Urinary incontinence is uncontrollable and involuntary urination, usually due to weak muscles around the urethra (the tube through which urine passes from the bladder out of the body). Urinary incontinence can be uncomfortable and cause you to limit your activities. Fortunately, urinary incontinence is usually treatable.
Types of Urinary Incontinence
- Stress incontinence – Occurs when coughing, laughing, picking up something heavy or exercising. Common in women, particularly after childbirth.
- Urge incontinence – Urgent desire to urinate with an inability to control the bladder.
- Total incontinence – Complete lack of bladder control.
- Overflow incontinence – Inability to empty the bladder because of an obstruction.
Diagnosis
- Urine tests
- Flexible viewing tube to see inside the bladder (cystoscopy)
- Urodynamic studies to test how well the bladder and urethra hold and release urine
Treatments
- Kegel exercises to strengthen the pelvic floor muscles
- Medications
- InterStim™ implanted device to control nerves that stimulate the bladder
- Botox bladder injections to relax muscles that cause frequent need to urinate
- Surgery
Surgery
- Transvaginal Bulking Up
- An FDA-approved biomaterial is injected into the urethra through the vagina
- The biomaterial narrows the urethra and strengthens it so urine cannot leak out
- Same-day procedure, does not require general anesthesia
- Recommended for young women who may want to have more children or older women who are not candidates for general surgery
- Transvaginal Sling
- Mesh is placed under the urethral sphincter (the muscles that control the exit of urine from the bladder) to reinforce it and stop the leakage of urine
- Just three small incisions are made in the vagina and at the pubic hairline
- Surgery under general anesthesia, patients spend one to three days in the hospital and recover within two weeks
- Recommended for women who are in good health and do not wish to have any more children
Urinary incontinence or “bladder control” issues can happen in women naturally as they age, as a result of childbirth, or as a side effect of a health condition or medication. Urogynecologists also treat interstitial cystitis, a chronic inflammation of the bladder.
- Symptoms
- Leaking or loss of bladder control
- Feeling the need to urinate frequently
- Inability to completely empty the bladder
- Pain in the lower abdomen, urethra or vagina
Interstitial cystitis is chronic inflammation of the bladder. It is not caused by bacteria and does not respond to antibiotics. It may be associated with other chronic conditions such as fibromyalgia, irritable bowel syndrome and endometriosis.
Symptoms
- Frequent urination
- Urge to pass urine immediately
- Pain in the lower abdomen, urethra or vagina
- Related symptoms include muscle and joint pain, migraines, allergic reactions and digestive problems
Diagnosis
- Urine tests
- Flexible viewing tube to see inside the bladder (cystoscopy)
- Bladder is distended with water during cystoscopy to check for small hemorrhages on the bladder wall
Treatments
While there currently is no cure for interstitial cystitis, treatments can help relieve the inflammation and symptoms and include:
- Medication
- Administering medications directly into the bladder
- Changes to your diet
- Stress management, biofeedback, bladder-strengthening exercises
- Electrical nerve stimulation
Why Choose Hackensack Meridian Health
- Fellowship-trained urogynecologists specialized in Female Pelvic Medicine & Reconstructive Surgery lead our program, ensuring advanced expertise and comprehensive care
- Extensive experience in minimally invasive and robotic surgery for urogynecology conditions provides patients with shorter recovery times and improved outcomes
- Full spectrum of care: from diagnostics (urodynamics, cystoscopy) to non-surgical therapies to reconstructive surgery—ensuring continuity and coordinated care within one system
- Convenient access across New Jersey’s regions with dedicated outpatient centres plus hospital affiliations, making advanced pelvic floor care accessible
- Patient-first approach: individualized treatment plans, clear communication, and supportive teams focused on restoring comfort, function and quality of life