I Think I Have Coronavirus, Now What?

March 13, 2020
Updated: 6/30/2020
If you think you’ve been exposed to COVID-19 or are developing symptoms associated with the illness, follow these steps to help protect yourself and others from getting sick.
If you’ve been exposed to someone who has tested positive for COVID-19:
Stay home and monitor your symptoms. COVID-19 causes flu-like symptoms including:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrhea
Avoid touching your face, nose and eyes and practice good hygiene such as washing your hands and cleaning “high touch” surfaces often
Avoid contact with others for at least 14 days even if symptoms have subsided.
If you exhibit symptoms:
Make a Call First
If you continue to experience mild symptoms including respiratory symptoms with fever and cough or if symptoms have worsened, you should utilize a telemedicine app or call your Primary Care Physician or nearest Urgent Care Facility.
- Using telemedicine instead of an office visit helps patients and caregivers avoid unnecessary exposure to COVID-19. Many physicians, including those at Hackensack Meridian Medical Group, now offer virtual office visits.
- For Urgent Care Facilities, you should call first for an initial phone consultation to screen for COVID-19 to avoid contact with other patients. Find a list of Hackensack Meridian Health’s Urgent Care locations here.
- If you have a primary care physician, please call their office for initial over the phone consultation as well. If you don’t have a primary care physician, you can locate one throughout Hackensack Meridian Health.
If a Visit is Required
If, after your initial phone consultation, the clinician advises you visit a care facility for further evaluation, please remember to call to let the facility know when you will be arriving. Caregivers in our patient care locations have rigorous precautions in place to reduce further spread of the virus either to other patients that do not have COVID-19 or the medical staff treating you.
When an Emergency Department Visit is Appropriate
If you are experiencing severe symptoms that you believe to be related to COVID-19, it is appropriate to go to the emergency department. Some emergency warning signs include*:
- Difficulty breathing or shortness of breath
- Persistent pain or pressure in the chest
- New confusion or inability to arouse
- Bluish lips or face
*This list is not all inclusive. Please consult your medical provider for any other symptoms that are severe or concerning.
For individuals who are high risk including those who are 65 or older and those who have compromised immune systems or are pregnant, seeking advice for your medical provider at the onset , regardless of symptoms is critical.
Our emergency departments are ready to deal with any emergency amid the coronavirus outbreak. We’re taking every precaution to prevent the spread of COVID-19 to patients who come to the emergency for severe or life-threatening illnesses.
If you are experiencing a life-threatening emergency, you need to call 9-1-1 and go to the emergency room.
Home Isolation
If your health care provider suspects you have a mild case of COVID-19, isolate at home. Here’s how:
- Restrict activities outside of your house, except for getting medical care as instructed by a health care professional. Don’t go to work, school or public places.
- Avoid public transportation, such as buses, taxis or other ridesharing options.
- Separate yourself from others at home. If possible, stay in a separate room and use a separate bathroom.
- Don’t handle pets or other animals while sick.
- Wear a face mask if you must be near other people (such as in a car or sharing a room).
- Always cover coughs and sneezes with your elbow or use a tissue. Throw the used tissue out in a lined trash can immediately and wash hands with soap and water (the right way) afterwards.
- Wash hands often for at least 20 seconds, using soap and water. If soap and water aren't available and your hands are not visibly dirty, use a hand sanitizer that contains at least 60% alcohol. However, if hands are visibly dirty, always wash hands with soap and water.
- Avoid sharing household items, such as dishes, cups and towels. Wash commonly used items often and thoroughly.
- Clean “high-touch” surfaces every day, such as counters, doorknobs, phones, keyboards and toilets. Use soap and water to clean surfaces and items that are visibly dirty, and then use an EPA registered household disinfectant. Always wear disposable gloves to clean and disinfect.
The decision to discontinue home isolation should be made in consultation with your health care provider and state and local health departments.
Monitor your symptoms
Take your temperature and check for symptoms daily. If your illness worsens, contact your doctor. We can’t stress enough how important it is to call before seeking care so the facility can properly prepare for potential exposure to COVID-19. You should continue to self-monitor for 14 days after exposure to the virus.
Help protect others in your household from getting COVID-19
When someone is on home isolation, it’s normal for others in the household to feel extra anxiety around contracting COVID-19. Follow these steps, in addition to those previously mentioned, to reduce the risk of spreading germs:
- While using a separate bathroom, if available, also use a separate bedroom.
- Restrict visitors who don’t have an essential reason for being in the home.
- Take the lead on caring for any pets.
- Make sure there’s good air flow in the home – using the air conditioner or opening windows if weather permits.
- Wear a disposable face mask and gloves if you have to come in contact with the patient, especially their blood, stool, saliva, mucus, vomit or urine. Throw away after using.
Next Steps & Resources:
- To make an appointment with a doctor near you, call 800-822-8905 or visit our website.
The material provided through HealthU is intended to be used as general information only and should not replace the advice of your physician. Always consult your physician for individual care.
Find a doctor near me
How to Take Care of a Loved One with Coronavirus

Care for a loved one with coronavirus? Learn essential steps for home care and protecting yourself. Get helpful guidance now.
6 Tips to Wash Your Hands the ‘Right’ Way

Learn proper handwashing techniques. Six simple steps for clean hands. Improve hygiene now.
Find a doctor near me
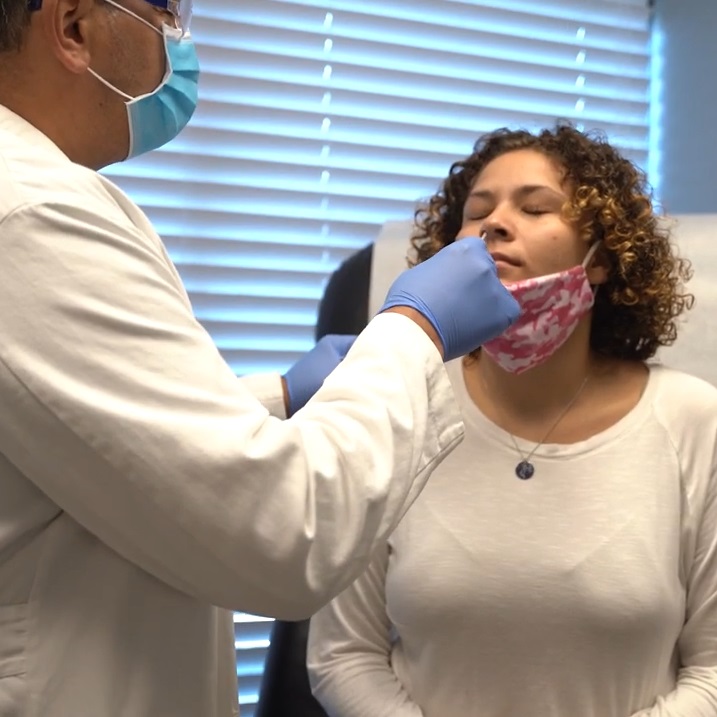
How to Prepare for a COVID Test
Prepare for your COVID-19 test. Find testing sites, learn what to bring, and avoid common mistakes. Get helpful tips for a smoother experience.

How to Prepare for Your COVID-19 Vaccine
Prepare for your COVID-19 vaccine. Learn how to schedule your appointment, what to wear, and what to bring. Get vaccinated today.

Can You Get COVID Twice?
Can You Get COVID Twice? Learn about COVID-19 reinfection from Drs. Nehmad and Unuigbe. Get the facts and stay safe. Call 800-822-8905.

Recovered from COVID-19? Why You Still Need a Vaccine
Dr. Thomas Bader has answered common questions about the COVID-19 vaccine that you may have if you’ve already experienced the illness
