CARF Accreditation at JFK Johnson Rehabilitation Institute
The Highest Level of Accreditation
 CARF accreditation is the gold standard of excellence and the highest level of accreditation possible for rehabilitation programs.
CARF accreditation is the gold standard of excellence and the highest level of accreditation possible for rehabilitation programs.
The following programs at JFK Johnson Rehabilitation Institute are accredited by CARF:
- Brain injury rehabilitation
- Acute Inpatient brain trauma unit
- Outpatient cognitive rehabilitation
- Extended Recovery Unit
- General inpatient rehabilitation
- Spinal cord injury
- Inpatient program
- Outpatient program
- Stroke rehabilitation
- Inpatient program
- Comprehensive Vocational Evaluation Services
What our CARF accreditation means to you
CARF® International is an independent, nonprofit organization that surveys and accredits more than 59,000 programs worldwide. CARF accreditation means that CARF surveyors have rigorously examined our services and operations to independently verify that each program strictly adheres to CARF’s internationally recognized standards of patient care and quality.
Our accreditation is also evidence of our commitment to:
- Involve you and your family with planning your care
- Provide you with treatment and services that will help you achieve the best outcomes possible
- Respect your cultural preferences
- Address public health and safety concerns, such as creating a culture of safety and emergency preparedness
- Maintain efficient, cost-effective management practices that are based on patient outcomes and satisfaction
- Remain accountable to our funding sources, referral agencies and the community at large
Answers to Frequently Asked Questions about Our Accredited Programs
Acute Brain Injury Specialty Program

The Acute Brain Injury Specialty Program directly provides medical, nursing and therapy services, including physical, occupational, speech and recreational therapy, as well as social work and psychology services.
Other services available onsite to all patients include medical consultations, diagnostic radiology services, laboratory services and pharmacy services, all available in Hackensack Meridian JFK University Medical Center.
The program does not provide services to patients who require a ventilator or for patients actively receiving chemotherapy.
The program delivers training and education services via information and communication technologies utilizing cell phone technology to the geographic areas that include the person served, their families, or their support systems.
Inpatient services at the Acute Brain Injury Specialty Program are provided 365 days per year, 24 hours a day, by rehabilitation nursing and physicians specializing in brain injury rehabilitation medicine.
Speech therapy, occupational therapy and physical therapy are provided 365 days a year, from 7 a.m. to 4:30 p.m. Therapeutic recreation therapy, Neuropsychology evaluation and rehabilitation psychology are provided based on individual patient needs.
Social workers serve as a liaison between the patient/family and the clinical treatment team and their services are provided five to six days per week between the hours of 8 a.m. and 5 p.m.
Other services available on-site to all patients in inpatient rehabilitation include medical consultations, diagnostic radiology services, laboratory services and pharmacy services, as available in Hackensack Meridian JFK University Medical Center.
All patients are scheduled for a combination of physical, occupational, and speech therapy three hours a day, five days out of seven, based on individual patient weeks. Therapy is usually not provided on the day of admission or discharge from the Institute. Social work, recreation therapy and rehabilitation psychology are provided five to six days per week, as needed, between the hours of 8 a.m. to 6 p.m.
After 90 days from discharge from JRI, 80 % of our patients reported the ability to perform self care activities (bathing, dressing, grooming, eating) was better than at the time of discharge, and 90% reported that the ability to move around at home was better than at the time of discharge.
Based on 2024 data from the follow up discharge survey.
Our goal is to return every patient back to his/her own home whenever possible. Most patients continue receiving follow-up therapy services after they’re discharged home. JFK Johnson Rehabilitation Institute has many opportunities for continued care, including a dedicated brain injury subacute program (the Extended Recovery Unit) and dedicated Outpatient Cognitive Rehabilitation program.

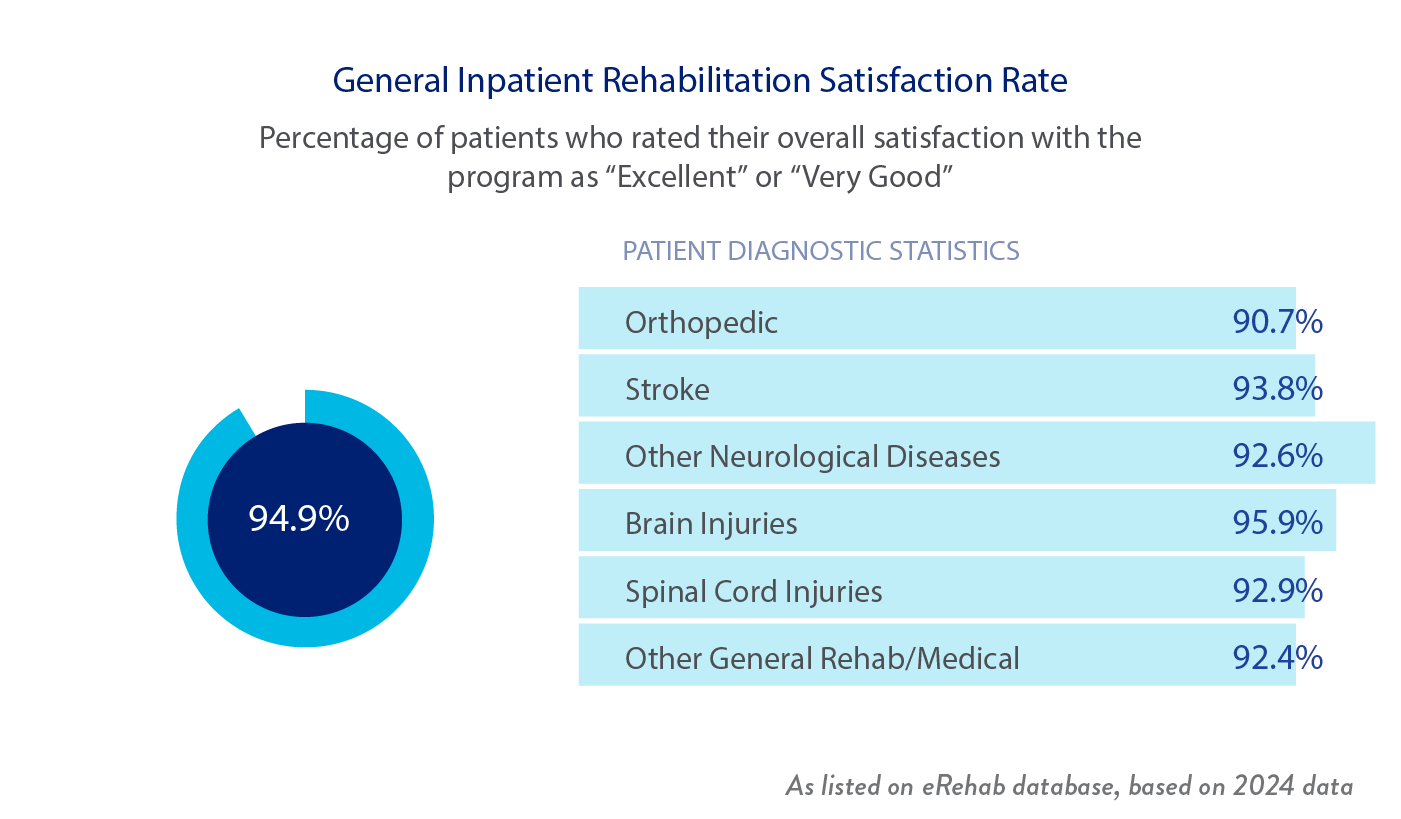
When a patient is discharged from the Institute, they receive a Patient Satisfaction Questionnaire. Patients answer the questions on a scale of 1-5 rating their satisfaction with program services in many areas. The highest rating is a score of 100%

Brain Injury Extended Recovery Unit

The Brain Injury Extended Recovery Unit, located in Hartwyck at Oak Tree, provides medical, nursing and therapy services, including physical, occupational, speech and recreational therapy, as well as social work, neuropsychology services and extensive group leisure activities, based on each patient's individual needs.
Inpatient services are provided 365 days per year, 24 hours per day, by rehabilitation nursing and physicians specializing in brain injury rehabilitation medicine.
Speech therapy, occupational therapy and physical therapy are provided Monday through Friday from 7 a.m. to 4 p.m. These services are provided 5 days per week, based on individual patient needs. Social work, recreation therapy and neuropsychology are provided five to six days per week, as needed, between the hours of 8 a.m. to 6 p.m.
Other services available on-site to all patients in inpatient rehabilitation include some medical consultations, diagnostic radiology services, laboratory services and pharmacy services. Those not available at the facility will be accessed at Hackensack Meridian JFK University Medical Center, which is located within 3 miles of the facility.
Patients receive approximately two hours of therapy, five days per week. It usually consists of physical therapy, occupational therapy, speech therapy and recreation therapy. Additional therapy groups and recreation groups are also available.
Our teams maintain extensive contact with families through phone calls, observing therapy sessions, and by participating in family training, family care plan meetings and family conferences.
We accept insurance payments from government-sponsored (Medicare and Medicaid) and third-party payers, including commercial insurances, workers’ compensation, motor vehicle insurance and private/self-pay. All insurances are verified for coverage prior to the initiation of services. Fees for services can be obtained through the Admissions Office.
We evaluate patients using the AM-PAC, which is a tool to assess functional outcomes and evaluate a person's ability to perform daily (or functional) activities important for independent living. Generally, our patients gain more independence and require significantly less assistance in performing important everyday tasks, such as moving around their home and out in the community, self-care, household chores and tasks that require attention, memory and thinking.

Our goal is to return patients back to their own homes with follow-up services whenever possible.

When a patient is discharged from the Brain Injury Extended Recovery Unit, they receive a Patient Satisfaction Questionnaire. Patients answer the questions on a scale of 1-5 rating their satisfaction with the program services in many areas. The highest rating is a score of 100%.

General Inpatient Rehabilitation FAQ
Adult patients with the following rehabilitation diagnoses are admitted to these units for treatment:
- Stroke
- Brain injury
- Spinal cord injury
- Amputations
- Neurological conditions
- Orthopedic conditions
- Cardiac conditions
- Other general medical/surgical conditions
The program does not provide services to patients who require a ventilator, are in a coma, require telemetry or who are actively receiving chemotherapy.
Patients who have an eligible admitting diagnosis may also have ongoing or new comorbid conditions.


We directly provide medical, nursing and therapy services, including physical therapy, occupational therapy, speech therapy and recreational therapy, as well as social work and psychology services, based on individual patient needs.
Other services available on-site to all patients in inpatient rehabilitation include medical consultations, diagnostic radiology services, laboratory services and pharmacy services, as available in Hackensack Meridian JFK University Medical Center.
Other services available to all patients every day in inpatient rehabilitation on site include:
- Medical consultations
- Diagnostic radiology services
- Laboratory services
- Pharmacy services
The program delivers training and education services via information and communication technologies utilizing cell phone technology to the geographic areas that include the person served, their families, or their support systems.
The inpatient rehabilitation program consists of three units, located on the first and third floors of JFK Johnson Rehabilitation Institute.
Inpatient services are provided 365 days per year directly at JFK Johnson Rehabilitation Institute, including 24 hours a day by rehabilitation nursing, and the availability of physicians specializing in rehabilitation medicine.
Speech therapy, occupational therapy and physical therapy are provided 365 days a year from 8 a.m. to 4:30 p.m.

After 90 days from discharge from JRI, 78.8% of our patients reported the ability to perform self care activities (bathing, dressing, grooming, eating) was better than at the time of discharge, and 81.3% reported that the ability to move around at home was better than at the time of discharge.
Based on 2024 data from the follow up discharge survey.
It is our goal to return every patient back to his/her own home, whenever possible. Most patients continue to receive follow up therapy services after they are discharged home.

When a patient is discharged from the Institute, they receive a Patient Satisfaction Questionnaire. Patients answer the questions on a scale of 1-5 rating their satisfaction with program services in many areas. The highest rating is a score of 100%.
Inpatient Spinal Cord Injury Rehabilitation FAQ
Individuals who have sustained a spinal cord injury (SCI), complete or incomplete, who do not require ventilator support. The etiology can be traumatic or non-traumatic, with or without comorbid conditions. If the SCI is attributed to a tumor, the individual must not receive concurrent chemotherapy during the inpatient admission.
Services include physical medicine, rehabilitation services, physical therapy, occupational therapy, recreation therapy, speech therapy, rehab psychology and a wheelchair clinic.
The following are the specific services we offer (all services provided directly unless specified):
- Medical/physiological: Abnormal tone, autonomic dysfunction, bladder function, body composition, bowel function, circulation, dysphagia, fertility (referred to specialist), infection management, medication, men’s health issues, musculoskeletal complications, neurological changes, nutrition, pain, respiration, sexual function (provided directly and/or referred to specialist), skin integrity and women’s health issues.
- Functional: Activities of daily living, assistive technology (provided directly and/or referred to specialist), behavior, cognition, communication, community integration, driving, durable medical equipment, emergency preparedness, environmental modifications, leisure and recreation, mobility, occupation, orthoses, personal care assistants (referrals made in conjunction with patient’s interests), prostheses and seating.
- Psychosocial: Adjustment to disability, behavioral health, substance use, family/support system counseling, peer support services and sexual adjustment.
- Education and training: Provided for the person served, families/support systems, the community and the professional community.
- Research capability: Ability to learn about current research and ability to participate.
- Transitions across the lifespan: Education and training provided by all team members on transitions through the lifespan based on areas of expertise.
- Case management: Available through the rehabilitation social worker and rehabilitation physician.
- Resource Management: Assistance available through rehabilitation social work.
- Follow-up: Physician and therapy follow-up services are recommended and/or provided directly.
- Health promotion and wellness: Education and training on introduction to health promotion and wellness available during inpatient stay and outpatient treatments; referrals to local activities available.
- Independent living and community integration: Provided through interactions with all team members.
- Prevention related to potential risks and secondary health conditions due to impairments, activity limitations, participation restrictions, and the environment provided through interactions with all team members.
- Safety for persons served in the environments in which they participate: Provided through interactions with all team members, and direct referrals to local community services.
The program delivers training and education services via information and communication technologies utilizing cell phone technology to the geographic areas that include the person served, their families, or their support systems.
Our comprehensive, integrated inpatient rehabilitation unit provides 24/7 nursing care and physician availability seven days per week. Rehabilitation nursing provides services continuously throughout the day.
Rehabilitation physicians generally see each patient a minimum of once daily.
We also provide a combination of physical, occupational and/or speech therapy for three hours daily, five days per week.
Social workers and recreation therapists are available Monday through Friday from 9 a.m. to 5:30 p.m., and for four hours on Saturday.
Rehabilitation nursing is available in the inpatient unit 24 hours/day, 7 days per week.
Rehabilitation physician services are available on the inpatient unit 24 hours per day, seven days per week.
The following services are available as needed on the inpatient unit, on an individualized schedule:
- Recreation therapy
- Rehabilitation psychology
- Medical consultations
- Nutrition counseling

After 90 days from discharge from JRI, 100% of our patients reported the ability to perform self care activities (bathing, dressing, grooming, eating) was better than at the time of discharge, and 100% reported that the ability to move around at home was better than at the time of discharge.
Based on 2024 data from the follow up discharge survey.
It is our goal for every patient to return to his/her own home whenever possible, where they typically continue receiving follow-up therapy services. For patients who were admitted with a diagnosis of SCI in 2022:

When a patient is discharged from the Institute, they receive a Patient Satisfaction Questionnaire. Patients answer the questions on a scale of 1-5 rating their satisfaction with program services in many areas. The highest rating is a score of 100%.

Visit our Spinal Cord Resource page for more information about preventing spinal cord injuries, aging and spinal cord dysfunction, support groups, research, employment, accessibility, and advocacy.
Inpatient Stroke Rehabilitation FAQ
We provide medical, nursing, social work and psychology services, physical therapy, occupational therapy, speech therapy and recreational therapy. Other services available on site through JFK University Medical Center to stroke patients include:
- Medical consultations
- Diagnostic radiology services
- Laboratory services
- Pharmacy services
- Education and training
- Risk management: Risk factors for stroke are identified and a plan to manage these controllable factors is implemented. These include diabetes, atrial fibrillation, hypertension and/or hyperlipidemia.
- Safety assessment, education and implementation: Safety for stroke patients includes individual adaptive safety measures and direct referrals to local community services upon discharge.
- Therapy: Focuses on addressing areas of limitation such as dysphagia (swallowing disorder), mobility, self care, speech/language, cognition, behavior and/or assistive technology. Considerations for post-discharge needs include smoking cessation, durable equipment needs, driver training, environmental/home modifications, leisure and recreation interests, occupation, orthoses and access to emergency care.
The program delivers training and education services via information and communication technologies utilizing cell phone technology to the geographic areas that include the person served, their families, or their support systems.
All patients are scheduled for three hours of therapy, five days out of seven. Therapy is usually not provided on the day of admission or discharge. Stroke patients are provided with 24/7 nursing care and physician availability. Social workers serve as a liaison between the patient/family and the clinical treatment team. All services are provided directly at JFK Johnson Rehabilitation Institute.
Referrals for outpatient or home care services are initiated at the time of discharge as well as the ability to transition to our Outpatient Stroke Recovery Program. Health promotion is emphasized and community reintegration is an area of focus in order to help Stroke patients be as independent as possible as they recover.


After 90 days from discharge from JRI, 75 % of our patients reported the ability to perform self care activities (bathing, dressing, grooming, eating) was better than at the time of discharge, and 75% reported that the ability to move around at home was better than at the time of discharge.
Based on 2024 data from the follow up discharge survey.
Our goal is to return patients back to their own homes whenever possible. Most patients continue to receive follow up therapy services after they are discharged home.

When a patient is discharged from the Institute, they receive a Patient Satisfaction Questionnaire. Patients answer the questions on a scale of 1-5 rating their satisfaction with program services in many areas. The highest rating is a score of 100%.

Outpatient Cognitive Brain Injury Rehabilitation FAQ
Clients have a wide range of needs and abilities following brain injury, ranging from requiring minimal assistance with higher level functioning to requiring more extensive treatment to address significant cognitive, emotional and physical limitations following severe brain injury or neurologic illness.

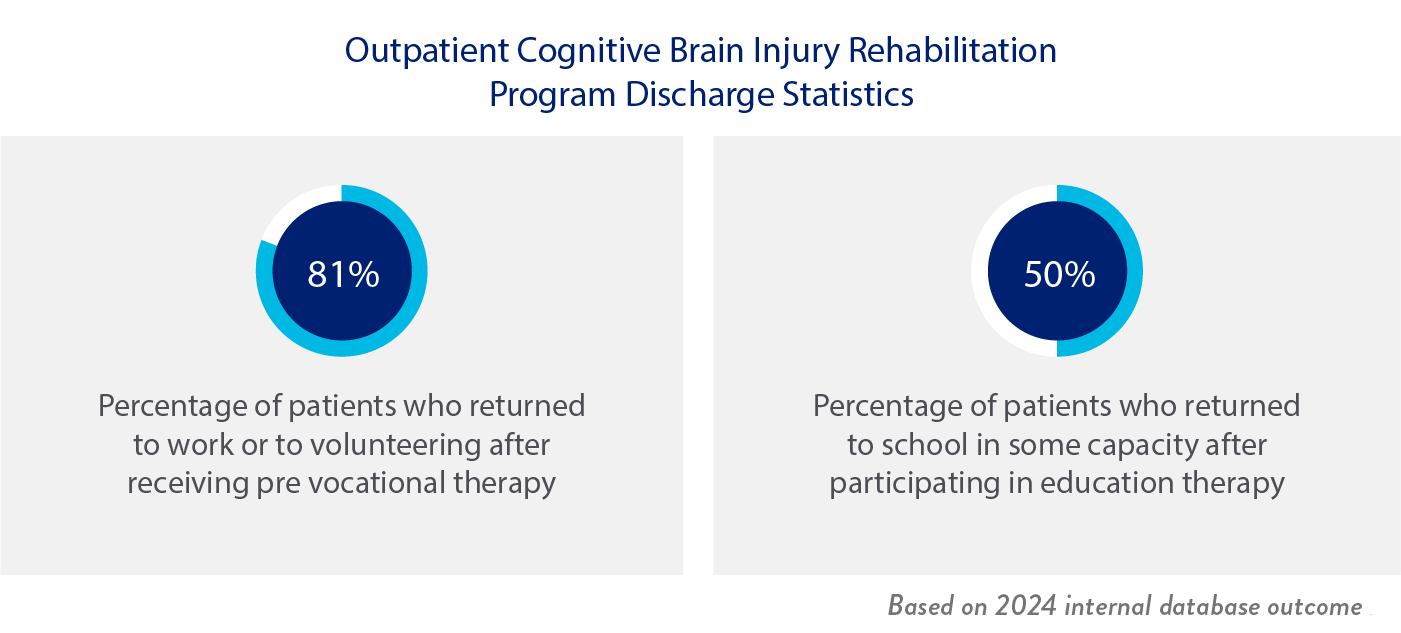
It varies greatly from person to person. Patients often return to work with requested accommodations, such as a gradual increase in work hours or job duties.
If a patient is returning to pre-injury employment, then the vocational therapists provide transitional support. Patients who are ready to return to work after therapy but do not have an existing job to return to, are referred to the Division of Vocational Rehabilitation for supported employment services.
Once students complete therapy, the education therapist helps with accommodation arrangements, as well as provides transitional support for students returning to high school or higher education.

Outpatient Spinal Cord Injury Rehabilitation FAQ

We directly provide physical and occupational therapy. Rehab medicine physicians, rehab psychology, wheelchair clinic, orthopedic clinic, and driver rehabilitation are also provided directly on site on an outpatient basis as indicated.
While this program is designed to help patients with a spinal cord injury, we do not provide these services to patients who are in a coma, undergoing chemotherapy or who require a ventilator or telemetry.
All services are provided directly at JFK Johnson Rehabilitation Institute:
- Outpatient physical and occupational therapy services are provided directly to the spinal cord patient population Monday through Friday, from 8 a.m. through 4:30 p.m.
Patients are seen two to three times per week depending on individual patient needs. Physical and occupational therapy is individualized-based on prescription and therapy evaluations. Most patients are scheduled for 2-3 visits per week, for 30-60 minute sessions.
The length of time in outpatient therapy depends on the severity of the injury and the individual’s progress. Since spinal cord injuries can involve long-term management of symptoms, patients can receive bouts of therapy throughout their lifetime.

All patients require a prescription for physical and occupational therapy.
We evaluate all patients upon admission to determine how much help they need to perform functional activities, such as walking, moving from lying down to sitting up, getting dressed, etc.

Upon discharge, therapists ensure that each patient has a thorough understanding of the recommended plan. Patients are always encouraged to follow-up with their referring doctor to assess future needs for therapy and to perform home exercise programs that were developed during their therapy sessions. Other referrals are made as needed, such as participating in a wheelchair clinic, orthotic clinic for bracing needs or spasticity clinic.
Patients are also referred to community activities such as wheelchair yoga, wheelchair basketball, support groups and peer mentoring programs.
When a patient is discharged from the Institute, they receive a Patient Satisfaction Questionnaire. Patients answer the questions on a scale of 1-5 rating their satisfaction with program services in many areas. The highest rating is a score of 100%.

Vocational Rehabilitation FAQ
The Vocational Rehabilitation Department serves adults and high school students in transition with disabilities. Our clients include persons with neurological impairments, physical disabilities, developmental disabilities, a psychiatric diagnosis, Autism Spectrum Disorders, vision loss and blindness, hearing loss and deafness and many other disabling conditions.
High school students may be accepted starting at age 15; under the IDEA, students may be eligible for services until the age of 21.
Adults are any person that is a high school graduate. There is no upper age limit for services. People of all ages are referred to first assess their vocational opportunities based on Interests, Aptitudes and Abilities. The Career Development Program for adults also offers a 60 day program. That provides our clients with the opportunity to try out or observe via observation, a wide range of occupations in a hospital and/or community environment. Clients are also provided with a paid work experience for 2 of the possible three months they are in program. Standard identifications such as Driver / non-Driver license and social security card required. Employee physicals are also provided.
Services are provided Monday through Friday from 9:30 a.m. to 5 p.m.
- Vocational evaluations are scheduled weekly for five or ten consecutive days within 14 days of receipt of referral information. Accommodations can be made on an individual basis.
- Career Development Program (adult & high school) operates generally between 9:30 a.m. to 2:30 p.m. Monday through Friday. Accommodations to schedules provided
- Training Programs occur with varying schedules, call for details.
The Department of Vocational Rehabilitation provides the following services directly onsite, including, but not limited to Vocational Assessment through:
- Achievement testing
- Interest inventories
- Dexterity testing
- Aptitude testing
- Perceptual testing
- Gross motor testing
- Situational assessments
- Career decision making inventories
- Career exploration
- Behavior observations
- Modes of communication
- Assistive technology and reasonable accommodations Needed
- Communication and other supports needed
- Interviews
- Learning styles
Other services offered by the Department of Vocational Rehabilitation are:
- High School Transition services, 5 hour and 3 hour programs
- Activities of Daily Living assessments/training (high school program)
- Work adjustment training
- Individual and group counseling for vocational needs
- Community-based mentorship
- Computer Application Training (CAT: Training in MS Office; 8th Grade Reading/Math required
Short-term vocational evaluations are conducted at JFK Johnson Rehabilitation Institute’s Vocational Rehabilitation Department in Edison. Situational assessments are in department worksites located on the JFK Johnson campus. On occasion, a situational assessment may occur in the community. Short-term evaluations are defined as five or ten days. School districts may request a 3 Day Vocational Evaluation to assist with student career planning.
The standardized assessments we use help to highlight your academics, interests and aptitudes.


There is a broad range of individuals served by vocational rehabilitation. High School students range from 15-21 years of age. Students come from many school districts. In addition to vocational and individual and group counseling, students participate in speech/communication groups. They have the opportunity to have lunch with their new friends/colleagues and often develop lasting relationships. Alumni activities are also sponsored. There is an equal number of males and females in the high school program with an average length of stay of 3 years.
The adult program is a shorter term program. A broad range of ages and people from all walks of life participate in the program for up to 60 days. Schedules may be 2-5 days weekly. Adults are served that may have experienced life-changing events such as injury that causes a change of career outlook.

We operate a program for high school students that provides vocational evaluations and allows students to participate in the “work study program” at JFK Johnson Rehabilitation Institute. Students are assigned a vocational counselor and an occupational therapist to work with them as they experience the year-round program. The program has historically demonstrated an equally high outcome rate for students that complete the program at or about age 21.

To be referred to JFK Johnson Rehabilitation institute’s Vocational Evaluation Services, you must be a client of the N.J. Division of Vocational Rehabilitation. They establish that you are a person with a need, and refer you to us. Last year our referral source gave us a 100% satisfaction rating with our services.
You can reach your county’s DVR Office by calling:
- Middlesex: 732-937-6300
- Union: 908-965-3940
- Somerset: 908-704-3030
If you live elsewhere, call us at 732-321-7069 and we will be happy to connect you with your local office.
You are also welcomed to visit us by appointment to see firsthand how our department works.


