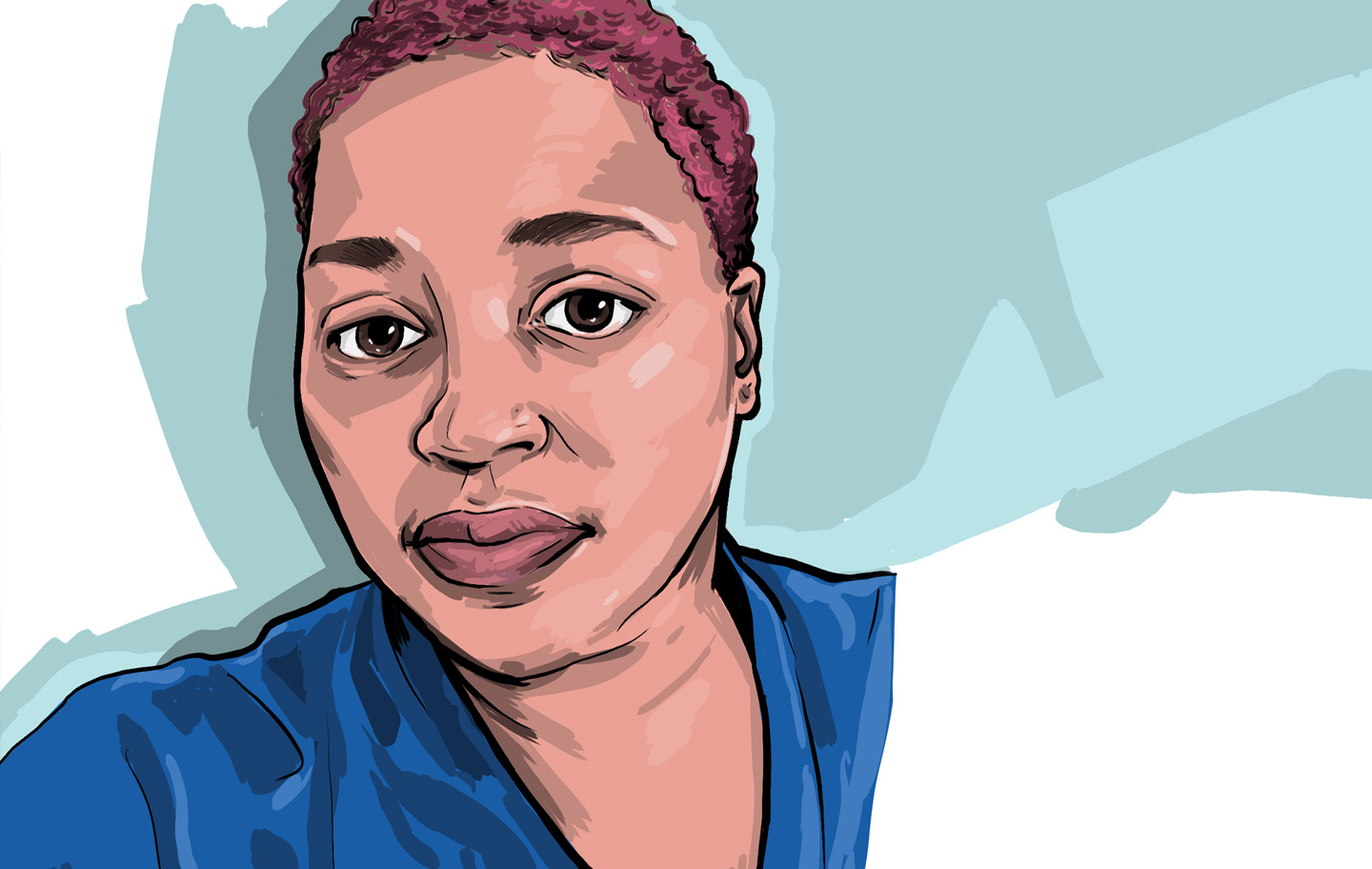
That was before he became one of them. In a highly unlikely twist of fate, Phillip, a nurse at JFK since 2015 and resident of Aberdeen Township, New Jersey, suffered a potentially catastrophic stroke at age 30 while working in the Stroke and Telemetry Observation Unit. What happened next not only reinforced the expertise and teamwork exemplifying JFK’s prestigious Stroke and Neurovascular Center, but ultimately offered Phillip invaluable insight about the neurology patients he cares for. By all accounts, his experience made him a better nurse.
“My curiosity, my questions kept growing. I had wondered what it’s like for patients to not be able to lift their arm after a stroke, or what it feels like to need a tube in your throat to breathe,” recalls Phillip, now 32. “I used to look at people with scars on their head and wonder what they went through. Today, I’m a stroke nurse who had a stroke in a stroke hospital—that’s why I’m alive.”
Colleagues Jump Into Action
It was Nov. 25, 2016—Black Friday—and the last hour of Phillip’s shift when disaster struck. Set to begin a coveted role the following Monday in a perioperative training program for nurses, he felt a headache come on. Seemingly typical at first, the pain progressively worsened to the point where Phillip, still finishing paperwork from his shift, placed an ice pack on his head.
“Then it got to the point where it was the worst headache I’ve ever had,” says the United States Coast Guard Auxiliary and bassoonist. “I texted that to my wife, and when I saw the words it was like a flashback to my nursing textbook to the section about hemorrhagic stroke.”
The vast majority of strokes, called ischemic strokes, are caused by clots in the blood vessels within the brain that hinder blood flow to vital cells. But hemorrhagic strokes, while less common, can be equally devastating. They occur when blood vessels in the brain leak or burst, leading to bleeding in or around the brain. Phillip had no idea he was born with a tangle of abnormal blood vessels connecting arteries and veins in the brain known as an AVM, or ateriorvenous malformation. His stroke occurred when his massive AVM ruptured.
Ten feet from the nurse’s station, “every symptom hit me at the same moment,” he explains. Dizzy, violently nauseous, and feeling his face droop and left side become paralyzed, Phillip urgently called out to his colleagues for help.
“The ER team was on the way up, and by the time the stretcher got to me I couldn’t function,” he says. “I felt someone throw me on the stretcher and I threw my phone to the secretary with my good hand and said, ‘Call my wife.’ The next thing I knew, it was Sunday.”
‘One-stop Shopping’ Enhances Recovery
For the next two days, gravely ill and connected to a breathing tube, Phillip received cutting-edge care in JFK’s Emergency Department and Neurocritical Care Unit. His brain was so swollen from the stroke that doctors performed surgery to stabilize the bleeding, placing the piece of skull bone removed during the procedure into a bone freezer for safekeeping. Phillip’s brain needed that extra space and time— free from the skull’s normal confines—to recover. “Otherwise the swelling, which continues to get worse for three to five days, almost certainly would have progressed to the point of brain death or permanent injury,” says neurologist Jawad Kirmani, M.D., director of the JFK Stroke and Neurovascular Center.
Phillip was clearly in the right place, since the facility is the first stroke center in the tri-state area designated as a Comprehensive Stroke Center by the Joint Commission. “The notion that ‘time is brain’ definitely applies in Phillip’s case,” Dr. Kirmani says. “He was extremely lucky his stroke happened on the stroke floor. Having such a devastating hemorrhagic stroke and coming out so intact had a lot to do with being in the right hospital where there was a stroke system in place for him to be taken care of rapidly.”
Awakened from heavy sedation, Phillip learned firsthand what it was like for a patient’s breathing tube to be suctioned and to not be able to fully move his left side. Vision impaired, he walked headfirst into a wall—a helmet protecting his soft spot—the first time he moved about with a walker. Physical and occupational therapists at JFK’s inpatient rehabilitation center worked intensively with him over the following weeks to help him recover and prepare for life at home, as well as for additional surgery.
“Every piece of my stroke recovery, until I came back to work, was all in that one building. The one stop shopping [feature] for neurology is incredible at JFK,” Phillip says. “If I’d had to transfer somewhere, it would have been so much harder for me and my family. I had direct access to my neurologist, my rehab doctors and everyone else in the same place. It makes the care so much easier and fluid.”
Bonding With Patients

Phillip regained his ability to move his left side before his next operation in January 2017, which paved the way for a near-complete recovery. First, Dr. Kirmani injected a glue-like material into tiny blood vessels around Phillip’s remaining AVM to “dry them out” before neurosurgeon Thomas Steineke, M.D., chairman of the JFK Neuroscience Institute, performed a lengthy operation to remove the mass and replace his skull flap.
More than two years later, the lingering physical effects from Phillip’s stroke are minor. He can’t see from the bottom left quarter in both eyes but is still able to drive, work and live normally. Learning new information is also harder than before, although Dr. Steineke notes, no one other than Phillip himself would notice.
“He has done phenomenally,” Dr. Steineke says. “The fact that he called his own stroke is amazing, but because he was so rapidly treated, it really preserved his brain function and allowed him to recover.”
“Certainly, Phillip immediately bonds with patients with similar conditions,” Dr. Steineke adds, noting that Phillip regularly assists him in the OR during neurosurgeries.
“I think he gives them hope you can have this very complex condition, undergo treatment and lead a full life.”
For his part, Phillip takes this new mentorship role very much to heart, participating in stroke advocacy events, happily explaining the story behind his scar and using his experience to enhance the care he gives patients. “One big rule about being a nurse, especially at bedside, is you should never say to a patient, ‘I understand,’ unless you’ve been there,” he says. “I know what it’s like to be a neuro patient. It helps you get through the hard cases, when you know you can connect with someone and help them feel better. I do have that piece now.”
Next Steps & Resources:
- Meet our source: Jawad Kirmani, M.D.
- To make an appointment with Jawad Kirmani, M.D. or another provider, call 800-822-8905 or visit our website
Find a doctor near me
Conquering Stroke